When you take antibiotics to fight a bacterial infection, these powerful medications don't just target the harmful bacteria causing your illness—they also affect the trillions of beneficial microorganisms living in your gut. Understanding how to effectively rebuild your gut flora after antibiotic treatment is crucial for maintaining optimal health and preventing long-term complications.
The human gut microbiome is a complex ecosystem containing over 1,000 different species of bacteria, along with viruses, fungi, and other microorganisms. This intricate community plays vital roles in digestion, immune function, mental health, and overall well-being. When antibiotics enter your system, they create significant disruption to this delicate balance.
Research published in Nature Microbiology demonstrates that even a short course of antibiotics can dramatically alter gut microbial composition. Studies tracking healthy adults over six months following antibiotic treatment revealed that the effects include initial blooms of potentially harmful bacteria like enterobacteria and depletion of beneficial species such as Bifidobacterium.
The impact varies depending on several factors:
One of the most common questions patients ask is: "How long does it take for gut flora to recover after antibiotics?" The answer is more complex than you might expect, and recent research provides sobering insights into the recovery process.
Studies indicate that while some bacterial populations begin recovering within days of completing antibiotic treatment, full restoration can take much longer. Research from UCLA Health suggests that it can take months or even years to recover the original species composition. In some cases, certain beneficial bacterial strains may never fully return to their pre-antibiotic levels.
The recovery process typically follows this pattern:
📅 Week 1-2: Initial recolonization begins, but potentially harmful bacteria may initially dominate
📅 Weeks 2-4: Beneficial bacteria start to re-establish, though diversity remains lower than baseline
📅 Months 1-6: Gradual improvement in microbial diversity, though some species may still be depleted
📅 6+ Months: Continued recovery, but some individuals may have permanently altered microbiomes
Your diet is the most powerful tool for rebuilding gut flora after antibiotics. Research consistently shows that dietary choices have a profound impact on microbiome recovery speed and effectiveness.
🌾 Increase Fiber Intake
High-fiber foods serve as prebiotics, providing fuel for beneficial bacteria. Focus on:
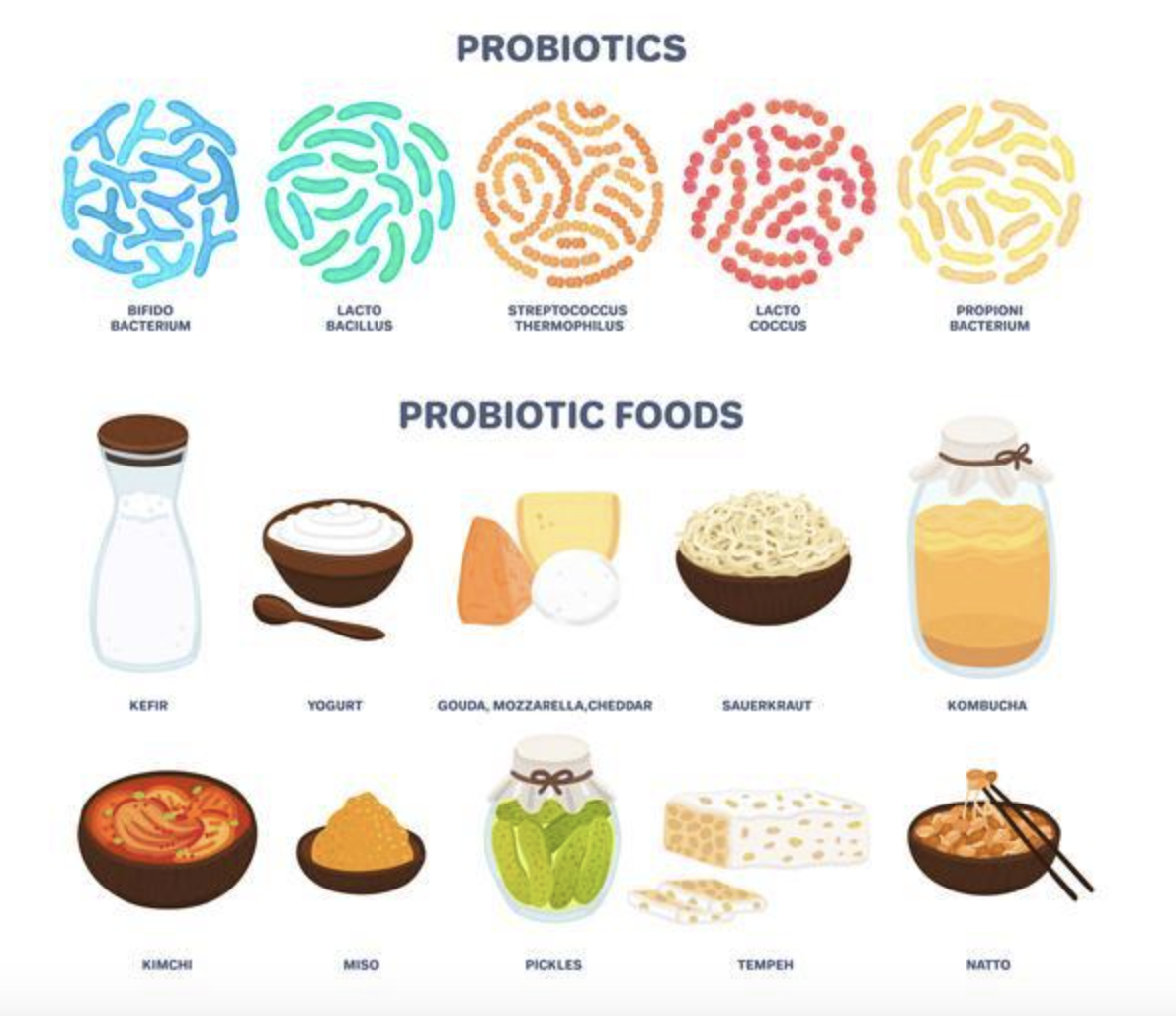
🥒 Incorporate Fermented Foods
Fermented foods naturally contain beneficial bacteria and can help seed your recovering microbiome:
❌ Limit Processed Foods and Added Sugars
Processed foods and excessive sugar can feed harmful bacteria and slow recovery. Focus on whole, unprocessed foods during your recovery period.
The role of probiotics in post-antibiotic recovery has been a subject of intense scientific debate, with recent research providing nuanced insights into their effectiveness.
📊 Current Evidence
A 2024 double-blind, randomized, placebo-controlled study published in Frontiers in Microbiomes examined the impact of probiotic supplementation on antibiotic-induced changes in the gut microbiome. While probiotics showed some benefits, the results were more complex than simple restoration of diversity.
However, a systematic review and meta-analysis published in BMC Medicine in 2023 challenged some assumptions about probiotic effectiveness. The research concluded that probiotic supplementation during antibiotic treatment may not be as beneficial for maintaining gut microbiome diversity as previously thought.
🏛️ The International Scientific Association for Probiotics and Prebiotics (ISAPP) Position
In December 2024, an expert panel concluded that more evidence is needed to determine whether probiotics help restore an antibiotic-disrupted microbiota. This doesn't mean probiotics are ineffective, but rather that their benefits may be more specific than previously understood.
✅ Practical Probiotic Recommendations
Based on current evidence, consider these approaches:
🧘 Stress Management
Chronic stress negatively impacts gut health and can slow microbiome recovery. Implement stress-reduction techniques such as:
🏋️♀️ Exercise and Physical Activity
Regular physical activity promotes gut health by:
Aim for at least 150 minutes of moderate-intensity exercise per week, including both cardiovascular exercise and strength training.
😴 Sleep Quality
Poor sleep can disrupt the gut microbiome and slow recovery. Prioritize good sleep hygiene:
Research published in Cell Host & Microbe highlights that recovery depends not just on individual interventions but also on environmental context. Factors that influence recovery include:
🏠 Household Microbiome Sharing
Living with family members or pets can help reintroduce beneficial bacteria through environmental sharing. This natural reseeding may be more effective than some artificial interventions.
🦠 Antibiotic Resistance Considerations
Antibiotic treatment doesn't just reduce beneficial bacteria—it can also promote the development and persistence of antibiotic-resistant genes in your microbiome. This resistome effect emphasizes the importance of judicious antibiotic use and thorough recovery protocols.
While food sources are ideal, specific prebiotic supplements may help accelerate recovery:
Some individuals may benefit from microbiome testing to:
However, it's important to note that microbiome testing is still evolving, and results should be interpreted by qualified healthcare professionals.
Consult with a healthcare provider if you experience:
Emerging research is exploring innovative approaches to microbiome restoration:
🔬 Fecal Microbiota Transplantation (FMT)
While primarily used for recurrent C. difficile infections, FMT research is expanding to other applications for microbiome restoration.
🎯 Precision Probiotics
Scientists are developing targeted probiotic therapies based on individual microbiome profiles and specific bacterial deficiencies.
⚗️ Postbiotics
These beneficial compounds produced by probiotics may offer some advantages over live bacteria supplements.
Developing an effective gut flora recovery strategy requires a personalized approach:
Rebuilding gut flora after antibiotics is a complex process that requires patience, consistency, and a science-based approach. While antibiotics can significantly disrupt your microbiome, the human gut has remarkable resilience and capacity for recovery when supported with appropriate interventions.
The key takeaways for successful gut flora recovery include prioritizing a diverse, fiber-rich diet, considering evidence-based probiotic supplementation, managing stress, maintaining regular physical activity, and being patient with the recovery process. Remember that individual responses vary, and what works best for one person may not be optimal for another.
As our understanding of the microbiome continues to evolve, new strategies and interventions will undoubtedly emerge. Stay informed about the latest research, work with qualified healthcare providers, and remember that investing in your gut health is an investment in your overall well-being.
The journey to restore your gut flora after antibiotics may take time, but with the right approach and commitment, you can rebuild a thriving microbial community that supports your health for years to come.